MEDIA
Originally By Victoria Buzz – July 5, 2016 – Click here to read original article Terrance Joseph Kosikar is 43-years-old and lives in the beautiful back-country mountains of British Columbia, Canada. On the opening day of the Vancouver 2010 Winter Olympics, a luge athlete by the name of Nodar Kumaritashvili, was killed during a training run at the Whistler...
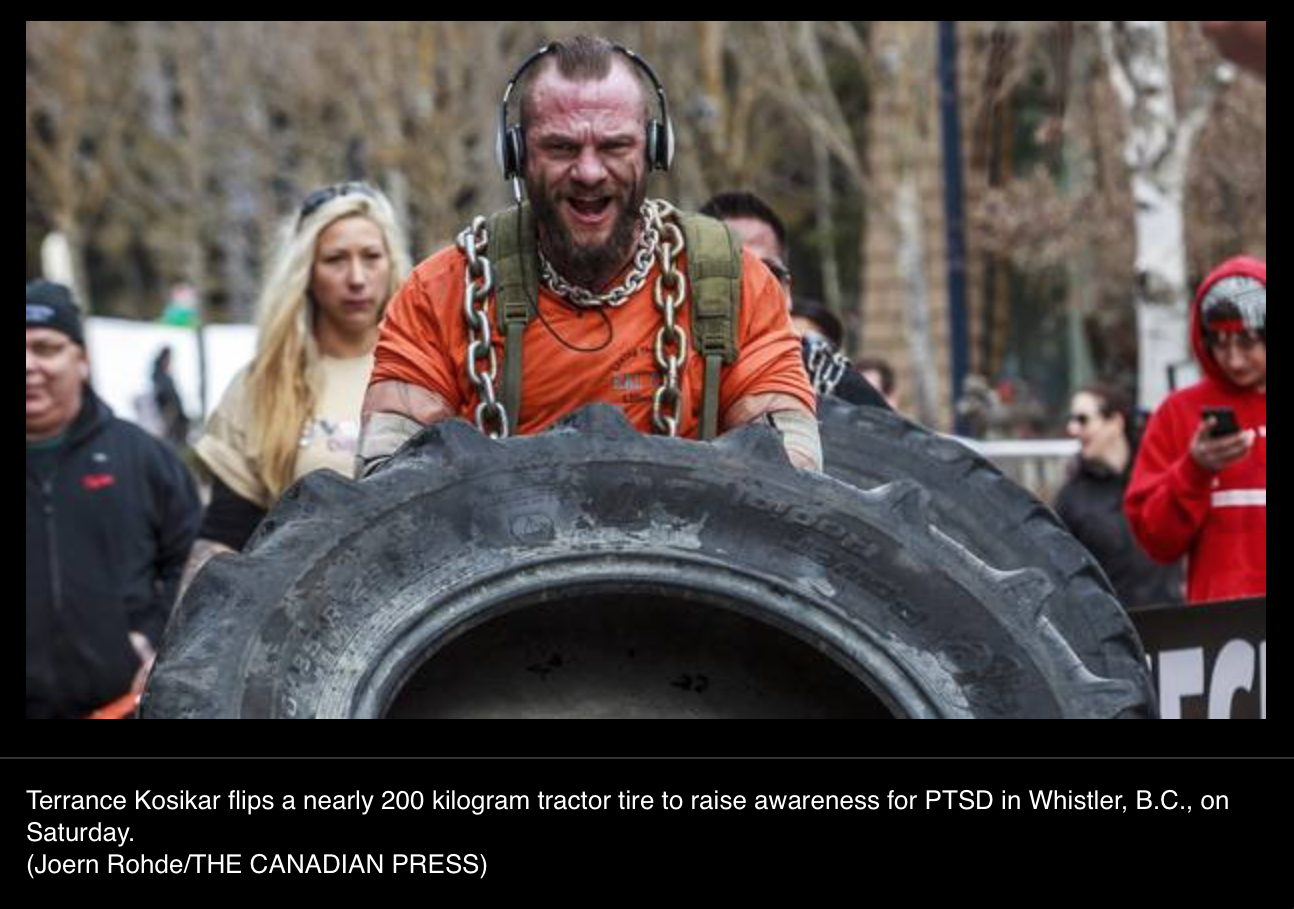
Originally published in The Globe & Mail here. Six years after the death of a Georgian luge athlete on the opening day of the 2010 Olympics, the first responder who tried to save him is still wrapped in the chains of post-traumatic stress disorder. On Saturday, Terrance Kosikar, 45, finished Breaking the Chains B.C.,...
Originally posted CTV News Vancouver here A British Columbia man who was the first responder to a horrific luge accident during the Vancouver 2010 Winter Olympics has finished a personal journey that he undertook in memory of the athlete who died. Terrance Kosikar arrived at the base of Blackcomb Mountain in Whistler on Saturday,...
So thankful! CTV News came to capture the start of my journey.

TERRANCE JOSEPH KOSIKAR
I was the first responder to a fatal accident at the Whistler Sliding Center on Opening Day of the Vancouver 2010 Winter Olympics. Although I was well trained in a myriad of life saving techniques, I was not prepared to deal with the emotional impact sustained while on the job. As a result of the fatality, I developed a Post-Traumatic Stress Injury that launched me into a very costly downward spiral. During several years of severe depression, anxiety, nightmares, and substance abuse, I lost my family, my career, and nearly my life. Pushed to my breaking point, I found salvation within. Escaping to the back-country near Lillooet, BC, I found peace and purpose in Mother Nature’s beauty and simplicity. Many others who have suffered from Post-Traumatic Stress have not been so lucky. By raising awareness and destigmatizing this debilitating mental injury, we can help the people suffering from Post-Traumatic Stress get the help they need.SPONSORS
Thanks to our many sponsors for their generous donations. Without them this would not have been possible!
We are currently editing this list. If your logo should be on here please contact the webmaster to be added.CONTACT
PAST EVENTS
Watch now – todays CTV news coverage live in English Bay, raising awareness to PTSD / Presumption of Illness petition. click here Terrance Joseph Kosikar’s heart rate went up, anxiety levels kicked in full throttle, just before speaking to over 40 men, at the Together We Can Drug and Alcohol Recovery and Education Society...
JULY 23 – 24th (11 am start) ENGLISH BAY – FIRST STEP HOPE FORMER BC FIRST RESPONDER RAISING AWARENESS TO PTSD by flipping a 400 pound tractor tire several kilometres while shackled in over 50 pounds of solid steel chain. On July 23rd- 24th,Terrance Joseph Kosikar will be flipping his tire in English Bay...
Meet a few Canadian First Responders and the Beautiful people of Canada who helped sign our petition during Canada Day. So far in the last week we have over 2000 signatures. Thank you Canada , we LOVE YOU.
**HUGE SUCCESS** at Magic Bike Ruedesheim Germany raising awareness to PTSD Together with – Two Capitols Chapter – Harley Owners Group Germany. Friday night, just before midnight and I had just laid down to bed when I heard the buzzzzzz from my cell phone. Yes, the Lion has a cell phone now, believe...
The Lion, peeks his heavy head out of his den this morning, eyes tired, back broken, knees and ligaments torn beyond repair. He grins and gently bears his teeth with a smile and a soft PRRRR. He looks up into the beauitful universe and is grateful for his strength he has been given to...
So thankful! CTV News came to capture the start of my journey.
Chapter 1: When the dark night Delivers the day Opening day of the Vancouver 2010 Winter Olympics Trust me when I say, I know this was very sad and heartbreaking video to watch, I have had to live with this hurt, loss and feeling for 6 long years. Yes, even still to this day I...
How to Help Someone with PTSD
Original article at www.helpguide.org can be seen here
When someone you care about suffers from post-traumatic stress disorder (PTSD), it can leave you feeling overwhelmed. The changes in your loved one can be worrying or even terrifying. You may feel angry about what’s happening to your family and relationship, or hurt by your loved one’s distance and moodiness. But it’s important to know is that you’re not helpless. Your support can make all the difference in your partner, friend, or family member’s recovery. With your help, your loved one can overcome PTSD and move on with his or her life.
Original article is at: https://www.helpguide.org/articles/ptsd-trauma/ptsd-in-the-family.htm
When someone you care about suffers from post-traumatic stress disorder (PTSD), it can leave you feeling overwhelmed. The changes in your loved one can be worrying or even terrifying. You may feel angry about what’s happening to your family and relationship, or hurt by your loved one’s distance and moodiness. But it’s important to know is that you’re not helpless. Your support can make all the difference in your partner, friend, or family member’s recovery. With your help, your loved one can overcome PTSD and move on with his or her life.
The impact of PTSD on relationships
PTSD can take a heavy toll on relationships. It can be hard to understand your loved one’s behavior—why he or she is less affectionate and more volatile. You may feel like you’re walking on eggshells or living with a stranger. You may have to take on a bigger share of household tasks, deal with the frustration of a loved one who won’t open up, or even deal with anger or disturbing behavior. The symptoms of PTSD can also lead to job loss, substance abuse, and other problems that affect the whole family. It’s hard not to take the symptoms of PTSD personally, but it’s important to remember that a person with PTSD may not always have control over his or her behavior. Your loved one’s nervous system is “stuck” in a state of constant alert, making him or her continually feel vulnerable and unsafe. This can lead to anger, irritability, depression, mistrust, and other PTSD symptoms that your loved one can’t simply choose to turn off. With the right support from friends and family, though, your loved one’s nervous system can become "unstuck" and he or she can finally move on from the traumatic event.6 tips for helping someone with PTSD
- Provide social support
- Be a good listener
- Rebuild trust and safety
- Anticipate and manage triggers
- Deal with volatility and anger
- Take care of yourself
Tip 1: Provide social support
It’s common for people with PTSD to withdraw from friends and family. While it’s important to respect your loved one’s boundaries, your comfort and support can help the person with PTSD overcome feelings of helplessness, grief, and despair. In fact, trauma experts believe that face-to-face support from others is the most important factor in PTSD recovery. How to support your loved one Knowing how to best demonstrate your love and support for someone with PTSD isn’t always easy. You can’t force your loved one to get better, but you can play a major role in the healing process by simply spending time together. Don’t pressure your loved one into talking. It can be very difficult for people with PTSD to talk about their traumatic experiences. For some, it can even make things worse. Instead, let them know you’re willing to listen when they want to talk, or just hang out when they don’t. Comfort for someone with PTSD comes from feeling engaged and accepted by you, not necessarily from talking. Do “normal” things with your loved one, things that have nothing to do with PTSD or the traumatic experience. Encourage your loved one to participate in rhythmic exercise that engages both arms and legs, seek out friends, and pursue hobbies that bring pleasure. Take a fitness class together, go dancing, or set a regular lunch date with friends and family. Let your loved one take the lead, rather than telling him or her what to do. Everyone with PTSD is different but most people instinctively know what makes them feel calm and safe. Take cues from your loved one as to how you can best provide support and companionship. Manage your own stress. The more calm, relaxed, and focused you are, the better you’ll be able to help a loved one with PTSD. Be patient. Recovery is a process that takes time and often involves setbacks. The important thing is to stay positive and maintain support for your loved one. Educate yourself about PTSD. The more you know about the symptoms, effects, and treatment options, the better equipped you'll be to help your loved one, understand what he or she is going through, and keep things in perspective. Accept (and expect) mixed feelings. As you go through the emotional wringer, be prepared for a complicated mix of feelings—some of which you’ll never want to admit. Just remember, having negative feelings toward your family member doesn’t mean you don’t love them.Tip 2: Be a good listener
While you shouldn’t push a person with PTSD to talk, if they do choose to share, try to listen without expectations or judgments. Make it clear that you’re interested and that you care, but don’t worry about giving advice. It’s the act of listening attentively that is helpful to your loved one, not what you say. A person with PTSD may need to talk about the traumatic event over and over again. This is part of the healing process, so avoid the temptation to tell your loved one to stop rehashing the past and move on. Some of the things your loved one tells you might be very hard to listen to, but it’s important to respect their feelings and reactions. If you come across as disapproving or judgmental, they are unlikely to open up to you again. Communication pitfalls to avoid Don't...- Give easy answers or blithely tell your loved one everything is going to be okay
- Stop your loved one from talking about their feelings or fears
- Offer unsolicited advice or tell your loved one what they "should" do
- Blame all of your relationship or family problems on your loved one's PTSD
- Invalidate, minimize, or deny your loved one's traumatic experience
- Give ultimatums or make threats or demands
- Make your loved one feel weak because they aren't coping as well as others
- Tell your loved one they were lucky it wasn't worse
- Take over your own personal experiences or feelings
Tip 3: Rebuild trust and safety
Trauma alters the way a person sees the world, making it seem like a perpetually dangerous and frightening place. It also damages people’s ability to trust others and themselves. Anything you can do to rebuild your loved one’s sense of security will contribute to recovery. Express your commitment to the relationship. Let the person know you’re here for the long haul so he or she feels loved and supported. Create routines. Structure and predictable schedules can restore a sense of stability and security to people with PTSD, both adults and children. That may mean help with groceries or housework, for example, maintaining regular times for meals, or simply “being there” for the person. Minimize stress at home. Try to make sure your loved one has space and time for rest and relaxation. Speak of the future and make plans. This can help counteract the common feeling among people with PTSD that their future is limited. Keep your promises. Help rebuild trust by being trustworthy. Be consistent and follow through on the things you say you’re going to do. Emphasize your loved one’s strengths. Tell your loved one you believe he or she is capable of recovery and point out all your loved one’s positive qualities and successes. Encourage your loved one to join a support group. Getting involved with others who have gone through similar traumatic experiences can help some people with PTSD feel less damaged and alone.Tip 4: Anticipate and manage triggers
A trigger is anything—a person, place, thing, or situation—that reminds your family member of the trauma and sets off a PTSD symptom, such as a flashback. Sometimes, triggers are obvious. For example, a military veteran might be triggered by seeing his combat buddies or by the loud noises that sound like gunfire. Others may take some time to identify and understand, such as hearing a song that was playing when the traumatic event happened, for example, so now that song or even others in the same musical genre are triggers. Similarly, triggers don’t have to be external. Internal feelings and sensations can also trigger PTSD symptoms. Common external PTSD triggers- Sights, sounds, or smells associated with the trauma
- People, locations, or things that recall the trauma
- Significant dates or times, such as anniversaries or a specific time of day
- Nature (certain types of weather, seasons, etc.)
- Conversations or media coverage about trauma or negative news events
- Situations that feel confining (stuck in traffic, at the doctor's office, in a crowd)
- Relationship, family, school, work, or money pressures or arguments
- Funerals, hospitals, or medical treatment
- Physical discomfort, such as hunger, thirst, fatigue, sickness, and sexual frustration
- Any bodily sensaton that recalls the trauma, including pain, old wounds and scars, or a similar injury
- Strong emotions, especially feeling helpless, out of control, or trapped
- Feelings toward family members, including mixed feelings of love, vulnerability, and resentment
- Tell them they’re having a flashback and that even though it feels real, it’s not actually happening again
- Help remind them of their surroundings (for example, ask them to look around the room and describe out loud what they see)
- Encourage them to take deep, slow breaths (hyperventilating will increase feelings of panic)
- Avoid sudden movements or anything that might startle them
- Ask before you touch them. Touching or putting your arms around the person might make him or her feel trapped, which can lead to greater agitation and even violence
Tip 5: Deal with volatility and anger
PTSD can lead to difficulties managing emotions and impulses. In your loved one, this may manifest as extreme irritability, moodiness, or explosions of rage. Understanding anger in PTSD People suffering from PTSD live in a constant state of physical and emotional stress. Since they usually have trouble sleeping, it means they’re constantly exhausted, on edge, and physically strung out—increasing the likelihood that they’ll overreact to day-to-day stressors. For many people with PTSD, anger can also be a cover for other feelings such as grief, helplessness, or guilt. Anger makes them feel powerful, instead of weak and vulnerable. For others, they try to suppress their anger until it erupts when you least expect it. Watch for signs that your loved one is angry such as clenching jaw or fists, talking louder, or getting agitated. Take steps to defuse the situation as soon as you see the initial warning signs. Try to remain calm. During an emotional outburst, do your best to stay calm. This will communicate to your loved one that you are “safe” and prevent the situation from escalating. Give the person space. Avoid crowding or grabbing the person. This can make a traumatized person feel threatened. Ask how you can help. For example: “What can I do to help you right now?” You can also suggest a time out or change of scenery. Put safety first. If the person gets more upset despite your attempts to calm him or her down, leave the house or lock yourself in a room. Call 911 if you fear that your loved one may hurt himself or others.Learning how to control anger
Anger is a normal, healthy emotion, but when chronic, explosive anger spirals out of control, it can have serious consequences on a person’s relationships, health, and state of mind. Your loved one can get anger under control by exploring the root issues and learning healthier ways to express their feelings. See: Anger ManagementTip 6: Take care of yourself
Letting your family member’s PTSD dominate your life while ignoring your own needs is a surefire recipe for burnout. In order to have the strength to be there for your loved one over the long haul, you have to nurture and care for yourself. Take care of your physical needs: get enough sleep, exercise regularly, eat properly, and look after any medical issues. Cultivate your own support system. Lean on other family members, trusted friends, your own therapist or support group, or your faith community. Talking about your feelings and what you’re going through can be very cathartic. Make time for your own life. Don’t give up friends, hobbies, or activities that make you happy. It’s important to have things in your life that you look forward to. Spread the responsibility. Ask other family members and friends for assistance so you can take a break. You may also want to seek out respite services in your community. Set boundaries. Be realistic about what you’re capable of giving. Know your limits, communicate them to your family member and others involved, and stick to them. Trauma can be "contagious" Caring for someone with PTSD can lead to the potential for secondary traumatization. You can develop your own symptoms from listening to trauma stories or being exposed to scary symptoms like flashbacks. The more depleted and overwhelmed you feel, the greater the risk that you may become traumatized.Support for people taking care of veterans
If the person you’re caring for is a U.S. military veteran, financial and caregiving support may be available. Visit VA Caregiver Support to explore your options, or call Coaching into Care at (888) 823-7458. For military veterans in other countries, see the Resources section below for helplines.Original article is at: https://www.helpguide.org/articles/ptsd-trauma/ptsd-in-the-family.htm